This is the first in my IVF series. You can also read about how we decided to go through IVF, how to chose a doctor, fresh versus frozen embryo transfers and working out during IVF.
Making the choice to start assistive reproductive treatments is no small task. It takes a lot of research, soul searching, communication, and questions, along with a big dose of patience and self-love.
While you may not feel you have a choice and that life has determined you need some help in order to have a baby, the ultimate decision is still up to you.

During and after the decision making process, you will have many questions and you may feel like you have very few answers.
Some of those questions will involve the IVF process itself.
Once you wade through the “what if’s” and “should we wait’s” and second opinions, you will want to learn all you can about what IVF actually entails.
Unfortunately there isn’t a lot of detailed information out there about what exactly happens during a typical IVF cycle.
While every cycle is unique depending on the patient, doctor and circumstances, there are many things that are similar about each IVF cycle.
By giving you this information and talking you through my experience with our cycles, I hope to give you a little peace of mind to make your planning and decision making less stressful.
What is IVF?
If you are here reading this I’m guessing you are somewhat familiar with what IVF does, but let’s do a quick review anyway.
In vitro fertilization (IVF) is a type of assistive reproductive technique. It involves using medication to promote egg growth and maturation in the woman. Then the eggs are collected during a surgical procedure called egg retrieval. The eggs are then placed in a safe and sterile environment in a lab. The husband’s sperm, which are usually collected the same day as the egg retrieval, are cleaned and washed and then placed in the same laboratory dish as the eggs in the hopes that the eggs are fertilized and grow to produce viable embryos.
If this happens, the embryos are transferred back into the woman’s uterus. If the procedure is successful, implantation and pregnancy occur.

There are many other forms of assistive reproductive techniques – such as IUI (intrauterine insemination) – but we were unable to try any of these due to our unique situation. I’ll talk only about IVF as that is what I know and have personally experienced.
Something Important to Remember
The first thing I want everyone going through IVF or considering IVF to know is that I don’t believe there truly is a “typical IVF cycle”. I read and listened to everything I could before starting IVF, and I still felt like I was in the dark once everything started. Each doctor’s appointment or test result brought new information I wasn’t quite prepared for, and new decisions that had to be made.
I had to throw my idea of “typical” out the window.
Please know that you are a unique individual and your body is completely unique. While your doctor will give you all of the advice they can on your first visit, they really won’t know everything about how you respond to the medication and the quality of your eggs until you go through a complete IVF cycle.
And even then, there may still be things that are simply a mystery.
IVF is an art as much as a science, and you have to be willing to do your own research, listen to your body, know yourself and communicate your feelings openly to your partner and doctor.
A Typical IVF Cycle and Calendar
While everyone is different, most reproductive endocrinologists will start first time patients on a very similar IVF protocol.
The basic components are these:
1. Ovarian suppression – usually birth control pills
2. Ovarian stimulation – this is the piece involving shots and what is typically referred to as “stimming”
3. Egg retrieval – a minor surgical procedure in which the woman is placed under anesthesia
4. Fertilization – happens in the lab
5. Embryo transfer – another procedure where a catheter like tube is placed up the woman’s vagina and into the uterus to place the embryos in the best spot for implantation (this is no more invasive or painful than a regular PAP smear, but it obviously holds a lot more emotional weight).
When you start and the actual timing of each phase will depend somewhat on your doctor and mostly where you are in your cycle.
It seems counter intuitive to be on birth control pills prior to starting IVF, but they are used to suppress the ovaries and pituitary gland. Your doctor basically wants everything under their control and on their schedule. They want to know EXACTLY what is going on in your body when you start the stimming medication, and the best way to do that is to kind of start from scratch. The birth control pill does that.
There is another protocol that uses Lupron injections instead of the pill to down regulate and suppress the ovaries. You will need to discuss the pros and cons of each with your doctor and see what is best for you. It’s possible they try one the first time and another the second time. We were offered the Lupron protocol for our second cycle and I planned on doing it until I found out we could NOT do a fresh embryo transfer if I used the Lupron in that capacity. So we opted out and stuck with our original protocol (with a few changes).
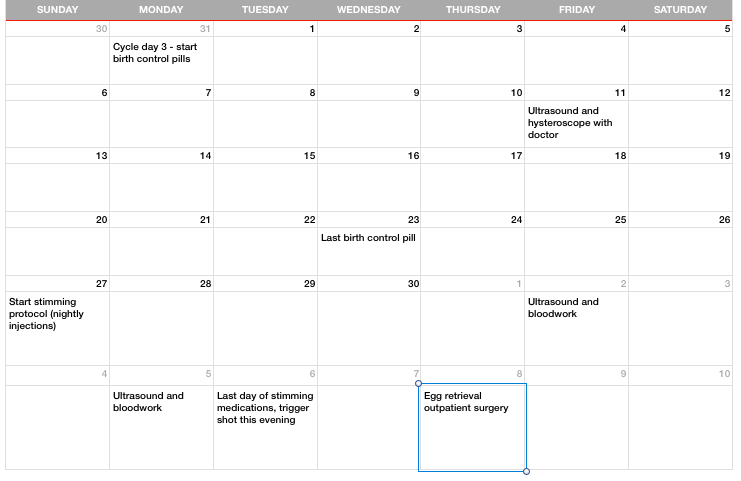
I’ll talk you through the protocol I followed for my first IVF cycle, which I have learned is very typical and common for most people during the first cycle. I’ll attach a calendar below as well so you can see it written out that way.
As I mentioned here, I first visited our doctor at the beginning of my cycle in October. I could have started then, but we weren’t quite emotionally ready. She gave me the prescription for birth control pills and told me to call them if I decided to start on my next cycle.
When I started my period again we knew we were finally ready, so I called my doctor and they told me to start the pill on day 3 of my cycle (day 1 of your cycle is the first day of your period).
I was on the pill for 24 days. Three days after stopping the pill, I started the ovarian stimulation medication. (You may or may not get some spotting or a regular period here. It just depends how you respond to the pill and it shouldn’t matter either way. I just got a little spotting but no period.)
The purpose of the ovarian stimulation part of the cycle is to stimulate your ovaries to produce eggs. The medication will first act on your follicle stimulating hormone to create more eggs. You will then add a GnRH-agonist (just another injection) to suppress the LH surge. In plain english, this means you are trying to grow eggs but NOT ovulate or release them yet.
I was on the stimulating injections for 10 days, and this is fairly typical. On the last day, you will stop the injections and perform what’s called the “trigger shot”.
This is an intramuscular injection of HCG (human chorionic gonadotropin) which causes the final maturation of the eggs.
The timing of the trigger shot is crucial. It has be given at an exact time so that it coincides with your egg retrieval, which will be two days after your trigger shot (my trigger shots were usually at 11:00pm/midnight so I could do an egg retrieval at 11:00am two days later).
During these 10 days you will be visiting your doctor quite a bit. I believe I went in for three different ultrasounds and at least as many blood draws. Your doctor will want to make sure the medications are doing their job of growing eggs but not allowing ovulation to occur. The ultrasounds also make sure you aren’t growing too many eggs, as this can lead to ovarian hyper stimulation syndrome.
Your doctor is looking for the perfect time to retrieve the eggs. This means they are mature and ready for fertilization but not past maturity.
The stimulation injections are subcutaneous, meaning just under the skin. All of mine were done in my belly. Each night at 9:00pm after our daughter was asleep we would meet around the kitchen island. He would lay out all the medication and needles and get everything ready (towards the end there were 5 shots a night, so it was quite the procedure). I would administer them myself, following the exact calendar our doctor had given us.
The trigger shot is a little different. It is an intramuscular injection, meaning it has to go all the way into the muscle. The most common spot for this is the buttocks. It is a big needle my friends, but honestly didn’t hurt any more than the others. I iced for 5 minutes before he did the shot and it was fine. It’s just not one that’s easy to do on your own and, because the timing is so crucial, it’s nice to have some help.
I can’t emphasize enough the importance of having SOMEONE with you during your injections. If you have a spouse or partner, I honestly think they should help in some way. I’m a control freak and even I appreciated having my husband be in charge of the needles and measuring and cleaning.

There are A LOT of moving pieces with all of the injections. Each one has a different needle and different dose. And the dose can change each day as well. Having someone there will help relax you and take some pressure off so you can just focus on your body. It also makes the entire thing more of a team effort, especially for women who sometimes feel alone going through their IVF journey.
All of the injections are done at home. You will have a long and in-depth injection training with your doctor or their assistant before all of this starts. I HIGHLY recommend having your partner or a friend there to review this with you. My husband wasn’t able to attend one of our two trainings, and I took pictures and videos and reviewed it with him right when I got home.
Don’t trust yourself to remember everything. Enlist help and support.
Common medications
Follistim or Gonal-F – These are the most commonly used stimulating medications to stimulate the ovaries to produce follicles and eggs (started on first day of stimming protocol).
Ganirelix or Cetrotide – These are the most commonly used medications to help prevent ovulation (started on day 6ish of stimming protocol).
HcG – “trigger shot”.
Omnitrope – Optional medication recommended by my doctor to help improve the quality of the eggs (I used this for 6 days on my first cycle and all 10 days of my second cycle. It is extremely expensive but, after doing research and considering my age and low egg count, my husband and I felt it was worth it).
What happens after the egg retrieval depends on many different things.
In a perfect world you would have the embryo transfer procedure done, but it could be done three days later, it could be done five days later or it could be done two months later.
This depends on whether you have opted to do a fresh or frozen transfer, your doctor’s protocol, how many embryos you have, your own personal decision and whether you are doing genetic testing.
These are all topics that can’t fit into a simple blog post, as they each have so much information and important issues surrounding them. My book about my own IVF journey and how you can navigate the IVF world will be released later this year and will include much more detail about each of these topics. You can sign up to learn more here.
In my next IVF series blog post I’ll talk about how to chose your doctor, as this is such an important decision. Not all doctors are created equal, and we will talk about the questions to ask that will help guide you in the right direction.
Remember, you are not alone! Join my email list here to stay up to date on everything I’ve learned about IVF. If you know someone going through this, please share it with them so they know they have a friend cheering them on.